Disclaimer: The content provided in this article is for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment. Medical technology evolves rapidly; always consult with qualified healthcare professionals regarding surgical options or rehabilitation plans suited to your specific medical condition.
The intersection of robotics and medicine has shifted from the realm of science fiction to the daily reality of hospitals and clinics worldwide. As of early 2026, robotics in surgery and rehabilitation represents one of the most significant leaps in the history of healthcare, fundamentally altering how procedures are performed and how patients recover from injury or illness.
For patients, families, and healthcare professionals, navigating this landscape can be overwhelming. The terminology is dense, the technology is complex, and the stakes—human health and mobility—are incredibly high. This guide aims to demystify the technology, explaining exactly how robots assist surgeons in the operating room and how they help patients relearn movement in the therapy gym.
Scope of this guide
In this guide, “robotics” refers to electromechanical systems that interact with the human body to assist, augment, or automate medical tasks. This includes:
- Surgical Robotics: Systems used during operative procedures to improve precision, visualization, and access (e.g., master-slave systems, autonomous guidance).
- Rehabilitation Robotics: Devices designed to assist people with disabilities or those recovering from trauma to practice movement and regain function (e.g., exoskeletons, end-effector devices).
Out of scope: We will not cover general hospital logistics robots (like those that carry linen or medicine down hallways) or purely pharmaceutical AI discovery tools, except where they directly interface with surgical or rehab hardware.
Key Takeaways
- Augmentation, not replacement: In 2026, surgical robots do not “perform” surgery on their own; they are sophisticated tools completely controlled by human surgeons to enhance precision and reduce invasiveness.
- Neuroplasticity is the goal: In rehabilitation, robots are primarily used to provide high-repetition, high-intensity therapy that drives the brain’s ability to rewire itself (neuroplasticity) after strokes or spinal cord injuries.
- Minimally invasive standard: The primary driver for surgical robotics is the ability to perform complex procedures through tiny incisions, leading to faster recovery times and less pain for the patient.
- Data-driven recovery: Modern rehab robots collect massive amounts of data on patient movement, allowing therapists to track progress with sub-millimeter accuracy and adjust treatment plans in real-time.
- Cost remains a barrier: While clinical outcomes are often superior, the high cost of acquisition and maintenance for these systems remains a significant challenge for widespread global adoption.
Part 1: Robotics in Surgery – Precision and Control
Surgical robotics has revolutionized the operating theater. Historically, surgery required large incisions to give the surgeon’s hands room to work and their eyes room to see. This “open surgery” caused significant trauma to the body, leading to long recovery times, high pain levels, and significant scarring.
The advent of laparoscopic (keyhole) surgery in the late 20th century improved this, but the instruments were rigid and difficult to manipulate—like trying to tie your shoelaces with chopsticks. Robotics solved this problem by reintroducing the dexterity of the human hand into a minimally invasive format.
How Robotic-Assisted Surgery (RAS) Works
Most major surgical robots today operate on a master-slave (or tele-manipulator) architecture. The robot does not make decisions; it translates the surgeon’s movements.
- The Console: The surgeon sits away from the operating table at an ergonomic console. They look into a stereoscopic viewer that provides a magnified, high-definition 3D view of the surgical site.
- The Interface: The surgeon places their fingers into master controls. When they move their hands, the robot moves its arms instantly and precisely.
- The Patient Cart: This component stands over the patient and holds the robotic arms. These arms carry the camera and the surgical instruments (scissors, graspers, cauterizers).
- EndoWrist Technology: Unlike straight laparoscopic sticks, robotic instruments have “wrists” at the tip. They can rotate 360 degrees and bend far beyond the range of a human hand, allowing for suturing and dissection in extremely tight spaces.
Key Types of Surgical Robots
While general soft-tissue robots are the most famous, the field has diversified significantly.
1. Soft Tissue Systems (General, Urology, Gynecology)
The dominant player here has long been the da Vinci Surgical System (Intuitive Surgical), though competitors have entered the market. These systems are used for:
- Prostatectomies: Removing the prostate with nerve-sparing precision to preserve function.
- Hysterectomies: Removing the uterus through tiny incisions.
- Cardiac Valve Repair: Fixing heart valves without cracking the chest (sternotomy).
- Colorectal Surgery: Operating deep in the pelvis where visibility is traditionally poor.
2. Orthopedic and Bone Systems
Unlike soft tissue robots that rely on the surgeon’s continuous control, orthopedic robots often use haptic boundaries and semi-autonomous cutting. Systems like the Mako SmartRobotics (Stryker) operate differently:
- Pre-planning: A CT scan is used to create a 3D model of the patient’s joint (knee or hip). The surgeon plans exactly how much bone to remove to fit the implant perfectly.
- Haptic Feedback: During surgery, the surgeon holds the robotic arm to cut the bone. If they try to cut outside the pre-planned safe zone, the robot physically resists or stops. This protects soft tissue, ligaments, and nerves from accidental damage.
3. Neurosurgical and Spine Systems
Precision is paramount when operating near the spinal cord or brain. Robots like the Mazor system function as ultra-precise guidance tools.
- Trajectory Guidance: The robot positions a guide arm based on pre-operative scans. The surgeon then drills or inserts screws through this rigid guide. This ensures that spinal screws are placed with sub-millimeter accuracy, reducing the risk of nerve damage.
4. Endoluminal and Single-Port Robots
Newer generations of robots are designed to enter the body through natural orifices (mouth, anus) or a single incision.
- Bronchoscopy Robots: These feature long, flexible, snake-like catheters that can navigate the complex airways of the lungs to biopsy tiny nodules that might be early-stage cancer, which manual tools cannot reach.
Benefits of Robotic Surgery
The value proposition of robotics in surgery is generally framed around the “Triple Aim” of healthcare: better experience for the patient, better health for the population, and lower cost per capita (though the cost factor is debated).
- Enhanced Visualization: The 3D magnification allows surgeons to see microscopic blood vessels and nerves clearly, preventing accidental damage.
- Tremor Filtration: The computer system filters out the natural physiological tremor of the surgeon’s hands. Even if the surgeon’s hand shakes slightly, the robot’s tip remains steady.
- Motion Scaling: The system can scale movement. A 5-centimeter movement of the surgeon’s hand can be scaled down to a 1-centimeter movement of the instrument, allowing for microscopic precision.
- Ergonomics: Surgeons can operate while seated, reducing fatigue during long procedures (some cancer resections can take 6–10 hours).
- Patient Outcomes: Generally, robotic surgery is associated with less blood loss, lower risk of infection, shorter hospital stays, and a quicker return to normal activities compared to open surgery.
Common Pitfalls and Limitations
Despite the hype, robotic surgery is not a magic bullet.
- Loss of Haptics: In most current soft-tissue systems, the surgeon cannot feel the tissue (haptic feedback). They must rely on visual cues (e.g., seeing the tissue deform) to judge tension. This requires a steep learning curve.
- Cost: A surgical robot can cost between $1 million and $2.5 million, plus high annual service contracts and expensive disposable instruments for every procedure. This limits access to wealthy or large academic hospitals.
- Setup Time: Docking the robot and preparing the arms takes time, though this has decreased with newer models.
- Latency: In telesurgery (operating from a distance), signal latency is a critical safety issue. Even a delay of 200 milliseconds can be dangerous.
Part 2: Robotics in Rehabilitation – Rewiring the Brain
While surgical robots focus on fixing acute issues, rehabilitation robots focus on restoring function lost to injury or disease. This field is heavily driven by the needs of an aging population and the prevalence of strokes, spinal cord injuries (SCI), and traumatic brain injuries (TBI).
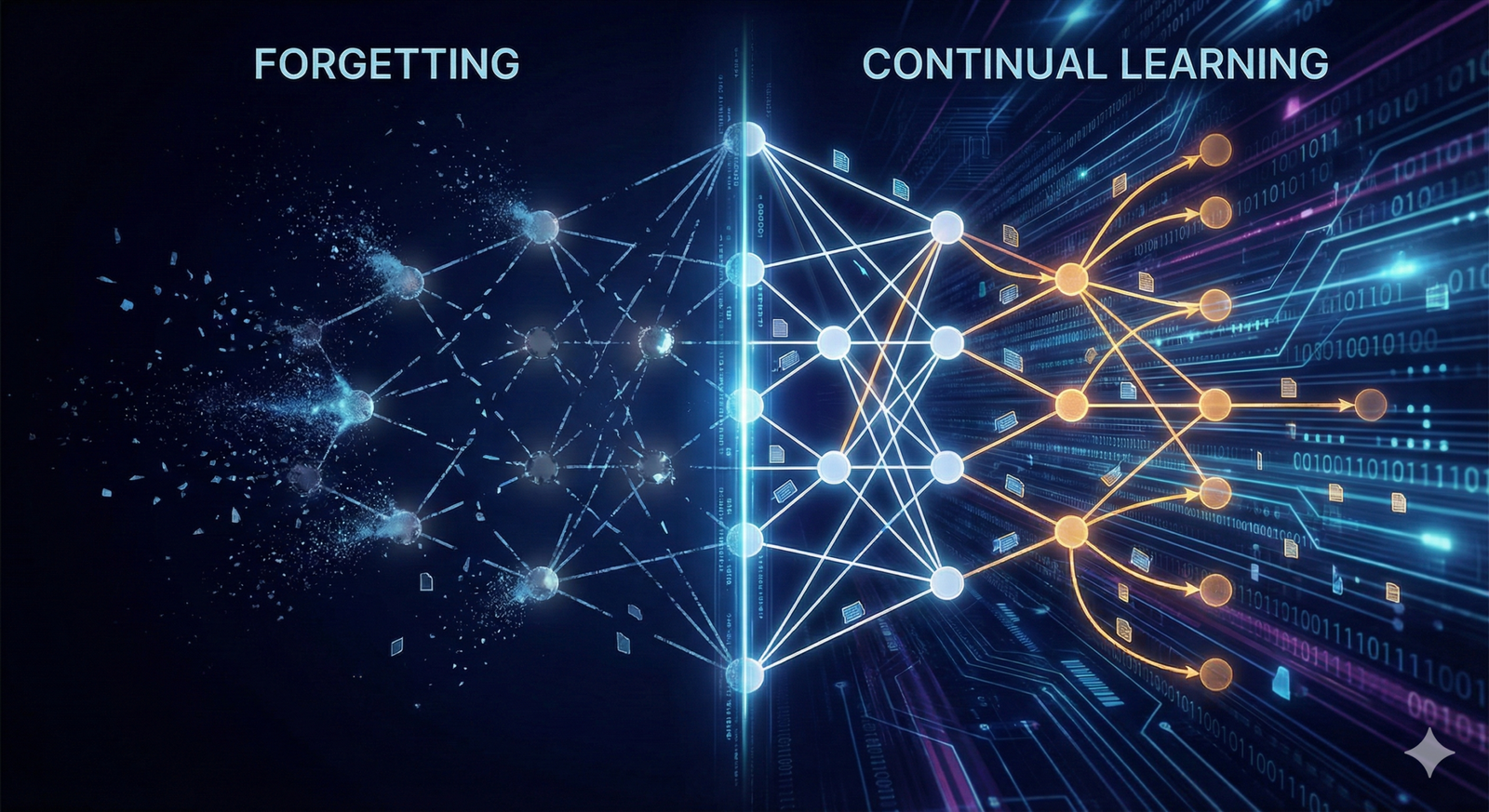
The core principle of rehab robotics is Neuroplasticity. The brain has the ability to rewire itself after injury, but this requires “massed practice”—thousands of repetitive, specific movements. A human therapist physically cannot guide a patient’s arm through 1,000 reaching motions in one hour without fatigue. A robot can.
Types of Rehabilitation Robots
1. Exoskeletons (Wearable Robots)
These are “suits” or braces strapped to the patient’s limbs. They use motors or hydraulics to move the joints.
- Lower Limb Exoskeletons: Devices like the Lokomat (a treadmill-based system) or the EksoNR (an over-ground wearable suit).
- How it works: The robot moves the patient’s legs through a perfect gait pattern.
- Use Case: Helping a paraplegic patient stand and walk, or helping a stroke victim relearn the rhythm of walking.
- Assist-as-Needed: Modern algorithms detect how much effort the patient is contributing. If the patient is weak, the robot does the work. As the patient gets stronger, the robot reduces assistance, forcing the patient’s muscles and brain to work harder.
- Upper Limb Exoskeletons: Devices like the ArmeoPower wrap around the arm and shoulder.
- Use Case: Restoring reaching and grasping functions after a stroke. These often incorporate gravity support, making the arm feel weightless so even weak patients can initiate movement.
2. End-Effector Systems
Unlike exoskeletons that align with the whole limb, end-effector robots connect only to the “end” of the limb (the hand or foot).
- Example: The InMotion arm robot. The patient holds a handle, and the robot moves the handle on a flat plane. The patient’s arm follows.
- Advantage: These are often simpler to set up and cheaper than full exoskeletons. They are excellent for shoulder and elbow recovery.
3. Soft Robotics in Rehab
A major trend in 2025–2026 is the shift toward soft robotics. Traditional exoskeletons are rigid and heavy. Soft robots use pneumatic artificial muscles or cable-driven gloves.
- Robotic Gloves: Soft, silicone gloves that inflate to curl the fingers. This helps patients with spasticity (clenched hands) open their hands to grasp objects, facilitating functional therapy like picking up a cup.
Gamification and Biofeedback
One of the distinct advantages of rehabilitation robotics is the integration of video games (gamification).
- The Problem: Doing 500 bicep curls is boring. Patients lose motivation.
- The Robotic Solution: The robot connects to a screen. The patient moves their arm to control a virtual character, catch virtual coins, or steer a virtual plane.
- Biofeedback: The system displays real-time data on the screen—showing the patient exactly how smooth their movement is or how much force they are exerting. This immediate visual reward loop is crucial for motor learning.
Evidence and Efficacy
Does it work better than human therapy? The research suggests:
- Dose-Response: Robots allow for a higher “dose” of therapy (more reps per session). Higher dose generally leads to better outcomes.
- Adjunct, not Replacement: Robots are most effective when used alongside conventional physiotherapy, not replacing it. The robot handles the heavy repetition; the therapist handles functional translation (teaching the patient how to use that recovered strength to dress themselves).
- Chronic Phase: Robots have shown surprising efficacy even in the “chronic” phase of stroke (6+ months post-injury), challenging the old belief that recovery plateaus after a few months.
Part 3: The Convergence of Technologies
The silos between surgery and rehabilitation are breaking down, driven by Artificial Intelligence (AI) and data connectivity.
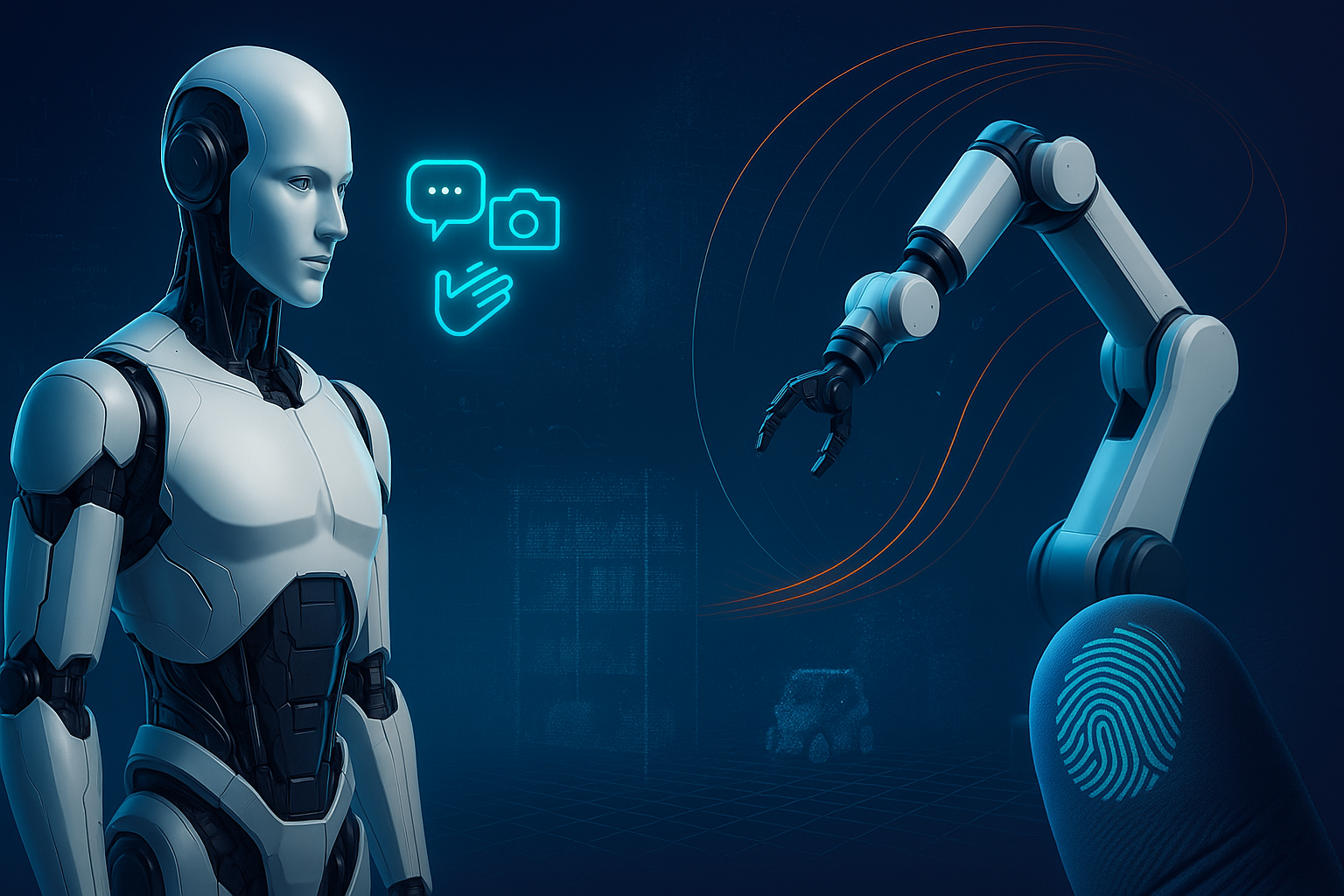
1. AI-Driven Surgical Planning and Guidance
In 2026, surgical robots are becoming “intelligent assistants.”
- Augmented Reality (AR) Overlays: Before cutting, the robot can overlay the patient’s MRI scan onto the live video feed. The surgeon sees the tumor “floating” inside the organ, allowing for “Superman vision.”
- Predictive Analytics: AI analyzes the video feed in real-time. If a surgeon moves an instrument too close to a critical artery, the system might flash a warning or provide haptic resistance to prevent a bleed.
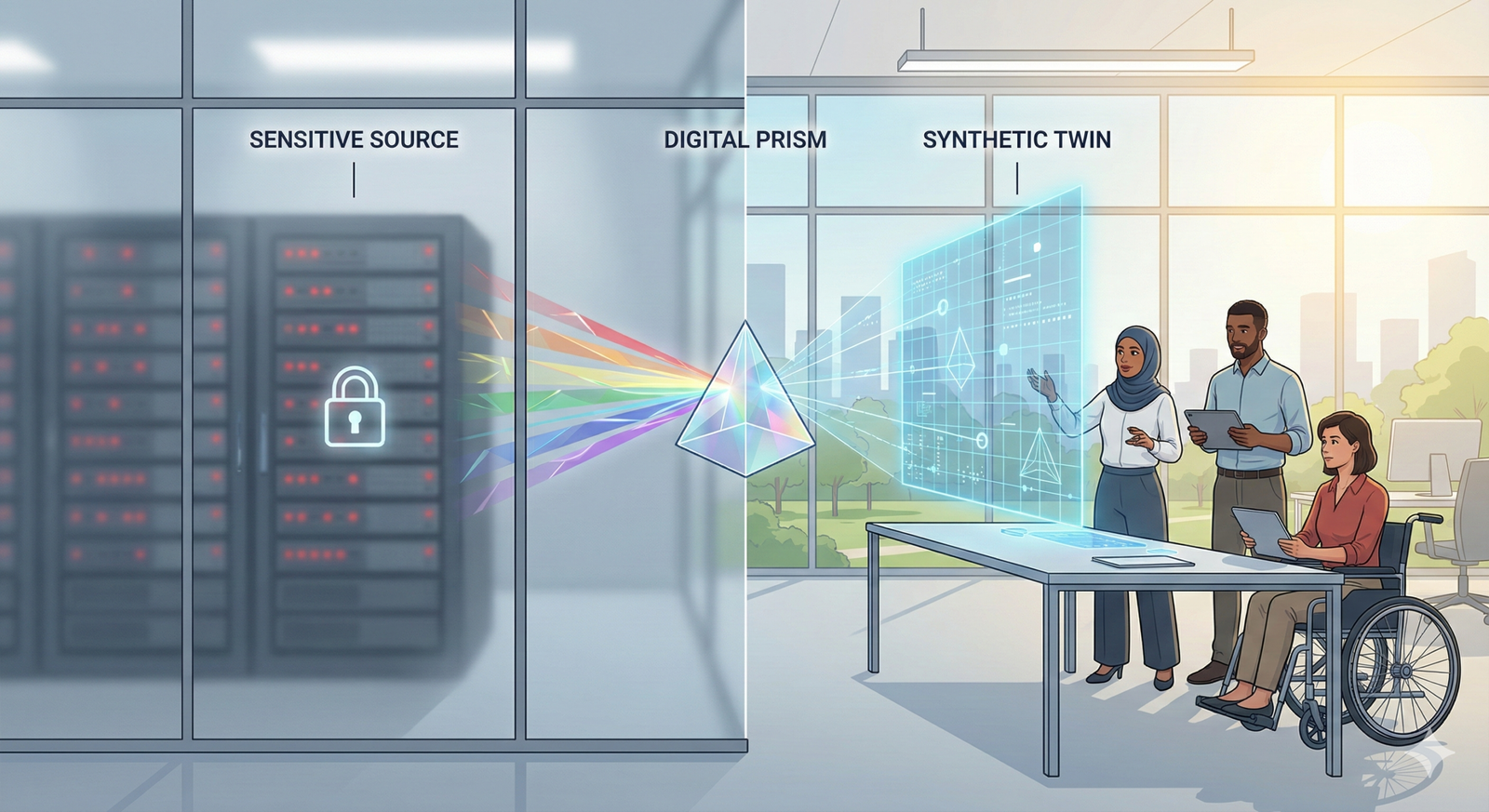
2. Digital Twins in Rehabilitation
Rehab robots are creating “Digital Twins” of patients.
- By analyzing the precise kinematics (movement angles, speed, smoothness) of a patient’s walk, the robot builds a digital profile.
- Therapists can compare this profile against thousands of other patients to predict recovery timelines and optimize therapy protocols. “Patients with this specific gait pattern recovered 20% faster when we focused on hip flexion.”
3. Telesurgery and 5G
The dream of operating from a distance is becoming a reality thanks to 5G and low-latency networks.
- Remote Expertise: A specialist in New York can “scrub in” virtually to assist a general surgeon in a rural clinic, guiding the robotic arms or controlling the camera.
- Humanitarian Missions: While fully remote surgery (surgeon in one country, patient in another) is still rare due to legal and latency risks, “telementoring” via robotic platforms is actively used to democratize access to high-level surgical skill.
Part 4: Ethical Implications and Challenges
As with any powerful technology, the rise of medical robotics introduces complex ethical and economic questions.
The Cost-Access Gap
The biggest criticism of medical robotics is that it drives up the cost of healthcare.
- Inequality: Hospitals in wealthy urban centers have multiple robots; rural or underfunded hospitals have none. This creates a two-tier system where the quality of your surgery or rehab depends on your zip code.
- Return on Investment (ROI): Hospitals are under pressure to use the robots constantly to justify the purchase price. This can lead to “indication creep,” where robots are used for simple procedures that could have been done just as well (and cheaper) via standard methods.
Liability and Autonomy
If a semi-autonomous robot makes a mistake—for example, if a bone-cutting robot malfunctions and cuts a ligament—who is responsible?
- The surgeon who oversaw it?
- The engineer who designed the algorithm?
- The hospital that maintained the device? Current legal frameworks generally pin liability on the surgeon (the “captain of the ship” doctrine), but as robots become more autonomous, this legal ground will shift.
The Human Touch
In rehabilitation, the emotional bond between therapist and patient is a key driver of recovery. There is a fear that “warehousing” elderly or injured patients in rooms full of automated machines could lead to social isolation. The consensus in the industry is that robots must remain tools for social interaction, not replacements for human care.
Who This Is For (and Who It Isn’t)
This technology is highly relevant for:
- Patients facing prostate, gynecological, thoracic, or orthopedic surgeries who want to explore minimally invasive options.
- Stroke or SCI survivors looking for intensive therapy options beyond standard manual stretching.
- Medical and Engineering Students looking to specialize in a high-growth field (Bioengineering, Mechatronics).
- Hospital Administrators evaluating the ROI of service line expansion.
This is likely not for:
- Emergency Trauma: Robotic surgery generally requires setup time. It is rarely used for gunshot wounds or car crash trauma where seconds count (though this may change).
- Minor Procedures: Robotics is overkill for minor surgeries like sewing up a superficial cut or removing a small skin tag.
Future Trends: What to Watch (2026–2030)
Looking ahead, three major trends define the future of this sector:
- Miniaturization (Nanorobotics): Moving beyond big arms, researchers are developing micro-robots that can travel through the bloodstream to deliver drugs directly to a tumor or clear a clogged artery from the inside.
- Autonomous Surgery: We are moving from Level 0 (no autonomy) to Level 1 and 2 (assistance and partial automation). By 2030, we may see robots independently suturing (stitching) wounds under human supervision, as suturing is a repetitive and tedious task.
- Home-Based Rehab Robotics: As technology shrinks and becomes cheaper, exoskeletons will move from the clinic to the living room. Patients will be able to “wear” their therapy for hours a day at home, dramatically increasing the intensity of rehabilitation.
Conclusion
Robotics in surgery and rehabilitation is no longer a futuristic concept; it is the current standard of care for many complex conditions. By enhancing human capabilities—giving surgeons “super” vision and steadiness, and giving patients “super” strength and endurance—these machines are reshaping the patient journey.
However, technology is only a tool. The most successful outcomes occur when these systems are integrated into a compassionate, human-centered care plan. Whether it is a da Vinci system reducing the trauma of a cancer operation or a Lokomat helping a paralyzed patient take their first steps in years, the robot is there to serve the human desire to heal and move.
Next Steps: If you or a loved one are facing surgery or rehabilitation, ask your provider specifically: “Is robotic assistance available for this procedure/therapy, and what are the specific benefits and risks for my case compared to traditional methods?”
FAQs regarding Medical Robotics
1. Is robotic surgery safer than traditional surgery? Generally, robotic surgery is considered as safe as traditional surgery, with the added benefits of smaller incisions, less blood loss, and faster recovery. However, like all surgeries, it carries risks, including potential mechanical failure (rare) or conversion to open surgery if complications arise. The surgeon’s experience with the robot is the most critical safety factor.
2. Does the robot perform the surgery by itself? No. In almost all current systems (as of 2026), the robot is fully controlled by the surgeon. It does not think or act on its own. The surgeon controls every movement of the robotic instruments via a console.
3. Will insurance cover robotic rehabilitation? Coverage varies significantly by region and provider. Many insurance plans cover the therapy session (e.g., “neuromuscular re-education”) regardless of whether a robot or human provides it. However, specific personal-use exoskeletons for home use are often not covered or require extensive appeals. Always check with your provider.
4. Can robotic exoskeletons help someone walk again after years of paralysis? It depends on the injury. For complete spinal cord injuries, exoskeletons can enable walking while wearing the device, providing health benefits like improved bone density and circulation. For incomplete injuries or stroke, they can be used as therapy tools to retrain the brain, potentially restoring some independent walking function over time.
5. How long does it take to recover from robotic surgery? Recovery is typically faster than open surgery. For example, a patient undergoing a robotic prostatectomy might go home the next day, whereas open surgery might require a week in the hospital. However, recovery timelines are highly individual and depend on the patient’s overall health.
6. What happens if the robot malfunctions during surgery? Surgical teams are trained for this specific scenario. The robot can be undocked (removed) from the patient in seconds, and the surgical team will convert the procedure to a traditional laparoscopic or open surgery to complete the operation safely.
7. Are surgical robots used for children? Yes, pediatric robotic surgery is a growing field. The precision and small scaling of robotic instruments are particularly beneficial for the small working spaces in children’s bodies, often used for urological or abdominal repairs.
8. What is “haptic feedback” and why is it important? Haptic feedback is the sense of touch (resistance, texture). Most current surgical robots lack this, meaning surgeons rely on vision to know how hard they are pulling on tissue. Newer generations of robots are beginning to incorporate sensors to restore this sensation, which helps prevent tissue damage.
9. Is robotic surgery more expensive? To the hospital, yes, due to the cost of the machine and instruments. To the patient, the cost is often similar to standard surgery if covered by insurance, but this varies. However, the total cost of care may be lower due to shorter hospital stays and fewer complications.
10. What is the difference between an exoskeleton and a prosthesis? A prosthesis replaces a missing body part (like an artificial leg for an amputee). An exoskeleton is a wearable device that wraps around an existing limb to provide strength, support, or movement to a paralyzed or weak limb.
References
- Intuitive Surgical. (2025). Da Vinci Surgical Systems: Technology Overview and Patient Information. Retrieved from https://www.intuitive.com
- Mayo Clinic. (2025). Robotic Surgery: What You Can Expect. Mayo Clinic Patient Care & Health Information. Retrieved from https://www.mayoclinic.org
- Stryker. (2024). Mako SmartRobotics for Total Knee, Total Hip, and Partial Knee. Retrieved from https://www.stryker.com
- Gassert, R., & Dietz, V. (2018). Rehabilitation robots for the treatment of sensorimotor deficits: a neurophysiological perspective. Journal of NeuroEngineering and Rehabilitation. Retrieved from https://jneuroengrehab.biomedcentral.com
- U.S. Food and Drug Administration (FDA). (2024). Computer-Assisted Surgical Systems (robotic technology). Medical Devices. Retrieved from https://www.fda.gov
- IEEE Robotics and Automation Society. (2025). Study Group on Medical Robotics: 2025 State of the Art Report. IEEE. Retrieved from https://www.ieee-ras.org
- Hocoma. (2025). Lokomat: Functional Locomotion Therapy. Retrieved from https://www.hocoma.com
- Ekso Bionics. (2025). EksoNR: Neurorehabilitation Exoskeleton Clinical Evidence. Retrieved from https://eksobionics.com