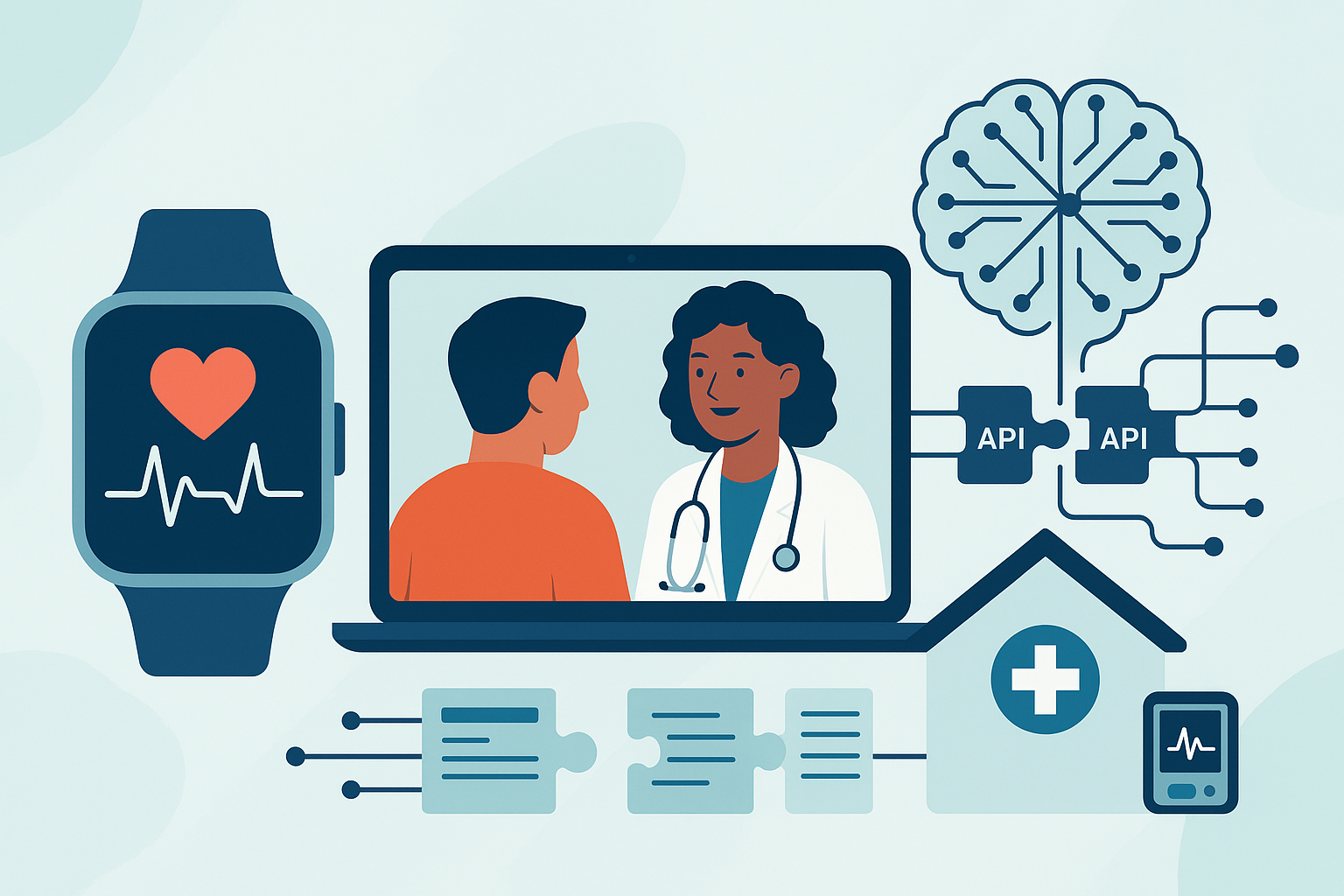
The future of care is arriving in your pocket, on your wrist, and across a growing web of secure, smart connections between home, clinic, and hospital. From wearables to telemedicine, five practical trends are redefining how patients engage with clinicians, how data flows, and how outcomes are measured. This article unpacks those trends in plain language and gives you detailed, starter-friendly steps to implement them responsibly.
Disclaimer: The information below is educational and not a substitute for professional medical, legal, or financial advice. For personal medical decisions and compliance questions, consult qualified professionals.
Who this is for: health system leaders, clinic managers, digital health teams, clinicians curious about virtual care and AI, and payer/provider innovators building the next phase of hybrid care.
What you’ll learn: the five trends to prioritize, step-by-step implementation, safety and compliance tips, what to track, common pitfalls, and a four-week starter plan you can run immediately.
Key takeaways
- Wearables + Remote Patient Monitoring (RPM) make continuous, real-world health data actionable and can reduce hospitalizations when programs are designed well.
- Telemedicine has settled into a durable role in hybrid care; start with visit types that clearly benefit from virtual workflows and build from there.
- AI at the bedside and in the back office (especially ambient documentation) can return time to clinicians—if you keep humans in the loop and measure results.
- Interoperability and open APIs turn data into a utility; align projects to current standards and national exchange frameworks instead of custom one-offs.
- Hospital-at-Home and advanced home diagnostics safely shift selected acute care to the living room when paired with rigorous protocols and connected tech.
1) Wearables & Remote Patient Monitoring (RPM)
What it is and why it matters
Wearables (watches, rings, patches) and connected home devices (BP cuffs, weight scales, pulse oximeters, glucometers) generate continuous or frequent signals about a person’s health between visits. When paired with an RPM program—structured enrollment, thresholds, triage, and follow-up—these data can surface deterioration early, personalize care plans, and reduce avoidable utilization. Global shipments of wearables reached the mid-500-million unit range in 2024, making the hardware ubiquitous and increasingly affordable (see References). Evidence syntheses show RPM can reduce hospitalizations and support better outcomes, especially in targeted conditions with clear escalation playbooks.
Core benefits
- Earlier detection of risk and exacerbations
- Tighter condition control and medication titration
- Potential reductions in admissions/readmissions and total cost of care
- Higher patient engagement via simple, at-home routines
- Clinician peace of mind through trend-based oversight instead of episodic snapshots
Requirements and low-cost alternatives
- Devices: validated consumer wearables and/or FDA-cleared home devices matched to your use case (e.g., hypertension, heart failure, COPD, diabetes).
- Connectivity: Wi-Fi or cellular hubs; for low-resource settings, choose devices with built-in cellular.
- Software: RPM platform to ingest device data, set thresholds, and route alerts; for low-cost starts, use vendor dashboards or CSV exports with manual triage.
- People: a small nurse/MA care team, a clinical champion, and a supervising physician.
- Governance: consent workflows, privacy/security controls, documentation templates, and clear clinical protocols.
Step-by-step implementation (beginner-friendly)
- Pick one condition and one outcome. Example: uncontrolled hypertension; aim for ≥10 mmHg average systolic reduction in 90 days.
- Define inclusion/exclusion. Start with motivated patients with smartphones or offer cellular devices; exclude patients without reliable access or those needing closer in-person monitoring.
- Choose 1–2 devices and a simple platform. Prioritize accuracy, ease of use, and battery life. Pilot first; don’t over-integrate on day one.
- Create a triage playbook. Thresholds (e.g., BP >180/120 twice in 15 minutes), who reviews, what messages go to patients, and when to escalate to telemedicine or in-person care.
- Train patients in 10 minutes or less. Hands-on first reading, written one-pager, and a helpline number or SMS keyword.
- Start with a 50-patient micro-pilot. Weekly huddle, rapid fixes, and protect the team’s time.
- Measure relentlessly. Enrollment, device adherence, alert-to-action time, average BP change, ED visits, readmissions, and patient-reported ease of use.
- Only then integrate with your EHR. After you’ve stabilized your workflow and KPIs, add single sign-on and discrete data ingestion.
Beginner modifications and progressions
- Simplify: Begin with a single device and a manual review hour daily.
- Progress: Add multi-condition bundles (e.g., BP + weight for heart failure), automated nudges, and predictive risk scoring.
- Scale: Move from one clinic to a service line; develop multilingual materials and loaner-device programs to improve equity.
Frequency, duration, and success metrics
- Frequency: Daily measurements for the first 2–4 weeks, then taper per protocol.
- Duration: 12-week episodes, renewable based on outcomes.
- KPIs: % days with readings, % patients active at 30/90 days, average change in clinical measures (e.g., systolic BP), 30-day readmission rate, ED visits per 100 members per month, patient satisfaction.
Safety, caveats, and common mistakes
- Alert fatigue from overly sensitive thresholds—pilot and adjust.
- Equity gaps from device, data, or language barriers—budget for cellular devices and multilingual support.
- Data overload without a triage playbook—assign roles and SLAs.
- Privacy/security lapses—use consent, PHI handling rules, and routine audits.
Mini-plan (RPM for hypertension — 3 moves)
- Enroll 50 patients with last-visit SBP ≥150; provide cellular BP cuffs.
- Daily readings auto-flag SBP >180 or <90; nurse calls within 30 minutes; schedule telemedicine adjustments within 48 hours if needed.
- Weekly pharmacist review for titration until 4 consecutive weeks within goal.
2) Telemedicine & Hybrid Care
What it is and why it matters
Telemedicine is now a permanent fixture in modern care. Utilization stabilized at about five percent of commercial claim lines in late 2024, with mental health dominating virtual visit categories (see References). Follow-up patterns for telehealth vs. in-person visits have remained comparable over multiple years across dozens of specialties, suggesting virtual care can safely replace many routine encounters when visit selection and workflows are clear. Several national flexibilities for coverage remain in effect through September 30, 2025.
Core benefits
- Expanded access and convenience
- Lower no-show rates when combined with reminders and easy links
- Faster first-contact resolution for simple issues
- Better continuity for behavioral health and chronic care check-ins
Requirements and low-cost alternatives
- Platform: a HIPAA-compliant video solution; for low-cost starts, use a vendor with bundled scheduling, reminders, and waiting rooms.
- Hardware: webcam, microphone, and lighting; patients need a smartphone or computer.
- Connectivity: test bandwidth; consider audio-only protocols when allowed.
- Workflows: virtual rooming, e-prescribing, lab/imaging orders, and a warm transfer path to in-person care.
Step-by-step implementation (beginner-friendly)
- Start with “virtual-fit” visit types. Behavioral health, medication refills, stable chronic disease follow-ups, minor acute concerns, and post-op checks.
- Script your virtual rooming. Confirm identity, allergies, vitals if self-reported, location for emergency purposes, and consent—every time.
- Stand up a “virtual front door.” Single link from your site/app to book or start a visit; reduce clicks and passwords.
- Route by protocol. Use triage questions to send urgent complaints to in-person or ED with clear red-flag scripts.
- Measure no-shows, cycle time, and follow-ups. Adjust schedules and visit lengths based on real data.
Beginner modifications and progressions
- Simplify: Start with daytime hours, two clinicians, and one specialty.
- Progress: Expand to after-hours urgent care with a rotating pool and protocolized triage.
- Scale: Add remote diagnostics kits (e.g., digital stethoscopes used by facilitators) and group visits for diabetes education.
Frequency, duration, and success metrics
- Frequency: Offer telemedicine daily during defined windows; publish those windows clearly.
- Duration: 10–20 minutes per routine visit; 30 minutes for complex follow-ups.
- KPIs: no-show rate, patient satisfaction, first-contact resolution, 7/30/90-day follow-up rates, and avoidable ED visits.
Safety, caveats, and common mistakes
- Emergency readiness: Always confirm the patient’s physical location; have escalation scripts.
- Licensure and coverage: Keep an updated grid; rules change and may differ by payer.
- Privacy: Prohibit using public Wi-Fi for PHI; use headphones in shared spaces.
- Scope creep: Don’t attempt complex new diagnoses without the right peripherals or an in-person plan.
Mini-plan (virtual urgent care — 3 moves)
- Offer 12–8 PM coverage daily with two clinicians; publish a symptom list appropriate for virtual.
- Add SMS reminders with a “join now” button; auto-route red flags to in-person care.
- Track 7-day bounce-backs and average wait time; refine staffing weekly.
3) AI in Care Delivery: Ambient Documentation & Decision Support
What it is and why it matters
AI is moving from pilots to the point of care—especially for ambient clinical documentation that listens during visits and drafts high-quality notes for clinician sign-off. At the same time, fully regulated clinical AI tools now number in the hundreds across imaging and other specialties. The promise is to cut clerical load, return time to patients, and standardize documentation quality—provided that humans remain firmly in the loop and outputs are audited.
Core benefits
- Reduce “pajama time” and after-hours charting
- Improve note completeness and consistency
- Speed up coding and downstream operations
- Free clinician attention for relationship-building and shared decision-making
Requirements and low-cost alternatives
- Use-case clarity: start with ambient documentation in one high-volume clinic.
- Technology: microphone hardware (often just a smartphone), ambient scribe software, EHR integration for drafts.
- Governance: PHI handling, consent language, model audit trail, and rollback plan.
- People: one clinical champion per site; a privacy/security partner; and an analyst to review time-savings and quality.
Step-by-step implementation (beginner-friendly)
- Pick one clinic and 3–5 clinicians willing to pilot; baseline their average note time and after-hours charting for 2 weeks.
- Deploy ambient capture with clear signage and verbal consent; ensure drafts are stored securely and labeled as AI-generated until signed.
- Establish a review rubric (accuracy, completeness, tone, billing elements). Require clinician sign-off on every note.
- Hold a weekly quality “stand-down.” Review 5–10 notes together; catalog errors; refine prompts and templates.
- Publish time-savings. Track average note time and after-hours minutes per day; retire the tool if it doesn’t help.
Beginner modifications and progressions
- Simplify: start with dictation/voice-to-text plus smart templates.
- Progress: add ambient AI for full narrative; then specialty templates (e.g., orthopedics, pediatrics).
- Scale: expand to inbox drafting and prior-auth letter generation with policy guardrails.
Frequency, duration, and success metrics
- Frequency: daily use during clinic hours.
- KPIs: average minutes per note, after-hours time, note quality scores, clinician satisfaction/burnout surveys, and coding completeness.
Safety, caveats, and common mistakes
- Hallucinations and omissions: always review and edit; never auto-sign.
- PHI risk: restrict who can access drafts; encrypt audio/text in transit and at rest.
- Over-automation: avoid decision support that bypasses clinical judgment; label AI assistance clearly.
Mini-plan (ambient documentation — 3 moves)
- Baseline: track two weeks of note times and after-hours work.
- Pilot: enable ambient capture for 4 clinicians; require sign-off and weekly audits.
- Decide: keep, fix, or end at 4 weeks based on predefined thresholds (e.g., ≥30% time reduction without quality loss).
4) Interoperability & Open Standards (APIs, Health Information Exchange)
What it is and why it matters
Data liquidity is becoming a utility. Modern APIs let patients retrieve their records in apps, clinicians exchange data across organizations, and payers automate prior authorization and care management. National exchange frameworks are maturing, creating a “network of networks” that reduces one-off interfaces and brittle point-to-point connections. The practical result: fewer information gaps and smoother transitions of care.
Core benefits
- Lower chart-chasing burden and faster care coordination
- Improved patient access to data and self-management tools
- Reduced friction for prior authorization and payer-provider workflows
- A foundation for analytics and machine learning built on standardized data
Requirements and low-cost alternatives
- EHR certification and APIs: ensure you expose modern endpoints for patient and clinician access.
- Data governance: a single data dictionary, API management, and app vetting.
- Exchange participation: connect to a national framework through an approved intermediary; for smaller clinics, join via your EHR vendor’s connectivity services.
Step-by-step implementation (beginner-friendly)
- Inventory your data flows. Map every interface and manual upload. Identify duplicates and custom HL7 messages that can become standardized API calls.
- Publish a read-only patient API. Test with your own portal/app; measure uptime and response times.
- Vet one third-party app (e.g., a home monitoring app) using a risk framework; document scopes and revoke procedures.
- Join a national exchange network through your vendor or a connectivity partner; verify that referrals, summaries, and labs can move seamlessly.
- Align to payer data rules. Plan your roadmap for required payer APIs and automation deadlines.
Beginner modifications and progressions
- Simplify: start with read-only patient access and basic document exchange.
- Progress: add clinician-to-clinician queries and referrals; implement write-back for common data (e.g., vitals, medications).
- Scale: onboard payer APIs to automate prior auth and coverage checks.
Frequency, duration, and success metrics
- Frequency: continuous operation; monitor 24/7.
- KPIs: API uptime, median response time, # of app authorizations, # of exchanged clinical summaries, turnaround time for records, and prior-auth cycle time.
Safety, caveats, and common mistakes
- Shadow integrations that bypass security policies—centralize access via API gateways.
- App sprawl without vetting—use an approval process and scopes.
- Stale endpoints—keep versioning and deprecation schedules.
Mini-plan (API first steps — 3 moves)
- Stand up read-only patient endpoints and publish a developer page with scopes.
- Pilot one third-party app with five volunteers from your patient advisory council.
- Connect to a national exchange via your vendor; verify record retrieval for 10 cross-org patients.
5) Hospital-at-Home (HaH) & Advanced Home Diagnostics
What it is and why it matters
Select acute care can now be delivered safely at home for well-screened patients using structured protocols, 24/7 virtual oversight, and in-home services. As of mid-2025, hundreds of hospitals across dozens of systems in many states are approved to provide HaH, and program coverage flexibilities are authorized through September 30, 2025. Studies and early federal analyses indicate HaH can achieve lower mortality, readmissions, and spending after discharge when implemented correctly, while patients report positive experiences.
Core benefits
- Hospital-level care without hospital-acquired risks
- Improved patient comfort and sleep
- Potentially lower costs and higher capacity for hospitals
- Smooth transitions back to primary care
Requirements and low-cost alternatives
- Command center: virtual nursing station with physician coverage.
- Home kit: cellular tablet, vitals devices, oxygen, and consumables; portable diagnostics agreements (mobile X-ray, phlebotomy).
- People: RN home visits, paramedic/tech support, courier partners.
- Connectivity: reliable cellular for homes without broadband.
- Protocols: inclusion criteria, escalation thresholds, and ED diversion procedures.
Step-by-step implementation (beginner-friendly)
- Start with one DRG group (e.g., COPD or heart failure) and tight criteria (stable oxygen requirement, reliable caregiver, safe home).
- Build a 24/7 escalation ladder. Nurse triage → on-call physician → dispatch paramedic → direct ED transfer when needed.
- Bundle services. Daily video rounds, scheduled vitals checks, medication administration, and rapid diagnostics.
- Track outcomes and costs vs. matched inpatients; use rolling cohorts.
Beginner modifications and progressions
- Simplify: begin with “hospital-at-home-lite” (enhanced home care post-ED) before full replacement of admission days.
- Progress: add more conditions and post-op pathways; add caregiver training and respite.
- Scale: negotiate payer bundles; integrate with community paramedicine.
Frequency, duration, and success metrics
- Duration: typical acute episode 3–6 days, with 30-day follow-up.
- KPIs: 30-day readmission, mortality, hospital-free days, patient satisfaction, adverse events, and cost per episode vs. inpatient.
Safety, caveats, and common mistakes
- Loose screening drives early failures—stick to criteria.
- Connectivity blind spots—default to cellular-enabled kits and offline protocols.
- Supply chain delays—pre-stage common items and define courier SLAs.
Mini-plan (HaH for COPD — 3 moves)
- Enroll stable COPD exacerbation patients meeting criteria; deliver kit and oxygen within 2 hours.
- Daily video rounds; nurse home visit on day 1 and as needed.
- Escalate per thresholds (SpO₂ drop, dyspnea scores); debrief every discharge within 72 hours.
Quick-start checklist (print and use)
- Pick one condition (RPM) and one visit type (telemedicine) to pilot.
- Name a clinical champion and a project owner; reserve 2 hours/week for a huddle.
- Create consent scripts for virtual care, AI assistance (if used), and home monitoring.
- Draft triage playbooks (thresholds, who responds, within what time).
- Stand up basic analytics: a weekly dashboard for enrollment, adherence, follow-ups, and outcomes.
- Confirm coverage rules and licensure; capture payer guidance in a one-pager.
- Test connectivity (clinic and patient homes); have audio-only and cellular fallbacks.
- Run a tabletop safety drill (emergency during a virtual visit; device breach; power outage at home).
Troubleshooting & common pitfalls
- Low device adherence: Simplify instructions; send reminders at the time patients normally measure (e.g., morning BP), and use loaner programs for those without devices.
- Alert overload: Raise thresholds, add “trend-over-time” rules, and triage in batches twice daily instead of real-time for non-critical signals.
- Televisit no-shows: Use SMS links that open directly in the app; offer a two-minute grace text; enable easy reschedule.
- AI note errors: Maintain a living “gotchas” list; adjust prompts/templates weekly and require explicit sign-off.
- Interop stalls: Stop building custom interfaces; switch to standard APIs and join a national exchange through your vendor.
- Equity gaps: Budget for cellular devices, multilingual scripts, and caregiver training; track outcomes by language/zip code and adjust.
How to measure progress (simple KPI scoreboard)
Access & engagement
- RPM enrollment rate
- % days with readings per patient
- Telemedicine no-show rate
Clinical outcomes
- Average SBP or HbA1c change over 12 weeks
- 30-day readmissions for targeted conditions
- Hospital-free days at 30 days (HaH)
Experience & operations
- Patient satisfaction (post-visit micro-survey)
- Clinician after-hours charting minutes/day
- Average time from alert to clinical action
Cost & efficiency
- ED visits per 1000 members per month (target population)
- Cost per HaH episode vs. inpatient matched controls
- Prior-auth cycle time (as interoperability matures)
A simple 4-week starter plan (for a mid-size clinic)
Week 1 — Pick & prepare
- Choose: hypertension RPM + behavioral health telemedicine + ambient documentation for two clinicians.
- Draft consents and triage playbooks; set up devices and the video platform.
- Baseline: measure note time and after-hours charting for pilot clinicians.
Week 2 — Launch micro-pilots
- Enroll first 25 RPM patients; daily checks noon/evening.
- Open telemedicine for 4 hours/day focused on follow-ups and refills.
- Enable ambient capture for two clinicians with daily sign-off and QA rubric.
Week 3 — Tighten the loop
- Hold a weekly quality stand-down: review alerts handled, any adverse events, note quality, and tele-routing errors.
- Fix thresholds, scripts, and device instructions; add multilingual materials.
- Publish your first dashboard and share wins and misses with staff.
Week 4 — Decide and expand
- RPM: if adherence ≥70% and SBP down ≥8–10 mmHg in early cohort, expand by +50 patients.
- Telemedicine: extend hours or add a specialty day if no-shows <10% and satisfaction ≥90%.
- AI: continue or pause based on ≥30% note-time reduction with maintained quality.
FAQs (quick, practical answers)
- Are wearable readings accurate enough to inform care?
Use validated devices and cross-check at the first visit. For clinical decisions, rely on trends and repeated measures rather than single readings. - What if patients don’t have Wi-Fi or smartphones?
Offer cellular-enabled devices or hubs and a phone-based workflow. Budget a pool of loaner kits. - How do we get reimbursed for RPM and telemedicine?
Coverage varies by payer and service; many programs reimburse RPM and virtual visits when documentation and frequency requirements are met. Keep a living reimbursement grid and update quarterly. - Can AI write notes without clinician oversight?
No. Treat AI outputs as drafts. Require clinician review and sign-off, and audit a sample weekly. - What visit types are poor candidates for telemedicine?
New, complex diagnoses requiring a detailed physical exam or procedures; anything with red-flag symptoms should default to in-person or emergency care. - How do we prevent alert fatigue?
Use condition-specific thresholds, combine rules (e.g., trend + symptom), and triage in scheduled batches unless there’s a critical alert. - What KPIs should we watch first?
Start with: % days with RPM readings, average telemedicine no-show rate, clinician after-hours charting minutes, and 30-day readmissions for your target condition. - Is Hospital-at-Home safe?
When run under strict inclusion criteria, standardized protocols, and 24/7 escalation, early analyses show favorable safety and outcomes. - What about privacy and consent?
Get explicit consent for virtual visits, AI drafting, and monitoring. Limit access to PHI, encrypt data, and conduct periodic security reviews. - Will interoperability projects take years?
Not if you start with read-only APIs and join a national exchange through your existing vendor. Expand once you see value. - How does 5G or better connectivity help?
Lower latency and more reliable links improve remote monitoring and video quality, especially for high-bandwidth peripherals. Always keep cellular fallbacks. - How do we show ROI?
Pair each trend with a specific financial metric (e.g., reduced no-shows, avoided readmissions, cost per HaH episode) and compare to a rolling matched control group.
Conclusion
The future of care won’t arrive all at once. It will arrive as a series of practical, well-scoped projects—smart wearables with simple playbooks, virtual visits where they make sense, AI that drafts but doesn’t decide, APIs that replace manual chasing, and acute care at home for the right patients. Start small, measure obsessively, and scale what works.
Call to action: Choose one trend from this article and launch your 4-week micro-pilot today—future-proofing your care starts with a single, well-designed step.
References
- Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices, U.S. Food & Drug Administration, updated July 10, 2025. https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-aiml-enabled-medical-devices-list
- Generalizability of FDA-Approved AI-Enabled Medical Devices for Clinical Use, JAMA Network Open, 2025. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2833324
- Generalizability of FDA-Approved AI-Enabled Medical Devices for Clinical Use, PubMed, 2025. https://pubmed.ncbi.nlm.nih.gov/40305017/
- Generalizability of FDA-Approved AI-Enabled Medical Devices for Clinical Use, PubMed Central, 2025. https://pmc.ncbi.nlm.nih.gov/articles/PMC12044510/
- Follow-Up Rates After Telehealth and Office Visits Steady in Last Three Years (PDF), Epic Research, January 9, 2024. https://media.epic.com/epicresearch/wordpressmedia/pdfs/follow-up-rates-after-telehealth-and-office-visits-steady-in-last-three-years.pdf
- Mental Health Conditions Ranked as the Number One Telehealth Diagnostic Category Nationally and in All Regions from July to December 2024, FAIR Health (press release), April 22, 2025. https://www.prnewswire.com/news-releases/mental-health-conditions-ranked-as-the-number-one-telehealth-diagnostic-category-nationally-and-in-all-regions-from-july-to-december-2024-302433617.html
- Telehealth Policy Changes After the COVID-19 Public Health Emergency, Telehealth.HHS.gov, updated March 20, 2025. https://telehealth.hhs.gov/providers/telehealth-policy/policy-changes-after-the-covid-19-public-health-emergency
- Telehealth, Medicare.gov, 2025. https://www.medicare.gov/coverage/telehealth
- Fact Sheet: Extending the Hospital-at-Home Program, American Hospital Association, July 2025. https://www.aha.org/fact-sheets/2024-08-06-fact-sheet-extending-hospital-home-program
- CMS Completes Initial Set of Participating Organizations in TEFCA (2024), Office of the National Coordinator for Health IT, 2024. https://www.healthit.gov/topic/interoperability/policy/trusted-exchange-framework-and-common-agreement-tefca
- CMS Interoperability and Prior Authorization Final Rule, Centers for Medicare & Medicaid Services, January 2024. https://www.cms.gov/priorities/key-initiatives/interoperability
- A Systematic Review of the Impacts of Remote Patient Monitoring Interventions on Safety, Adherence, Quality-of-Life and Cost-Related Outcomes, PubMed Central, 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11258279/
- Efficacy of Remote Health Monitoring in Reducing Hospitalizations, PubMed Central, 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11437225/
- Worldwide Wearable Device Shipments Are Forecast to Grow 6.1% in 2024 to ~538 Million Units, Business Wire (IDC release), December 16, 2024. https://www.businesswire.com/news/home/20241216855749/en/Wearables-to-Face-Continued-Growth-While-Giving-Way-to-New-Form-Factors-According-to-IDC
- Worldwide Shipments of Wearable Devices Grew 8.8% Year-Over-Year in Q1 2024 to 113.1 Million Units, Business Wire (IDC release), June 4, 2024. https://www.businesswire.com/news/home/20240604813697/en/Worldwide-Shipments-of-Wearable-Devices-Grew-8.8-Year-Over-Year-in-Q1-2024-While-Average-Selling-Prices-Continue-to-Decline-According-to-IDC
- 5G Datasets and 5G Healthcare Applications: A Comprehensive Review and Trend Analysis, Electronics (open-access journal), January 2024. https://www.mdpi.com/2079-9292/13/1/155
- Rejoyn™ Prescription Digital Therapeutic: 510(k) Summary (K231209) (PDF), U.S. Food & Drug Administration, 2024. https://www.accessdata.fda.gov/cdrh_docs/pdf23/K231209.pdf